Rapid Interpretation of EKGs⁚ A Comprehensive Guide
This guide offers a comprehensive overview of rapid EKG interpretation, a crucial skill for healthcare professionals․ We’ll explore the fundamentals of EKG interpretation, delve into key components and common abnormalities, and examine how to recognize cardiac ischemia and infarction․ We’ll also cover the role of EKG in emergency medicine, advanced interpretation techniques, and real-world case studies․ This guide is designed to empower you with the knowledge and skills needed for confident and accurate EKG interpretation․
Introduction to EKG Interpretation
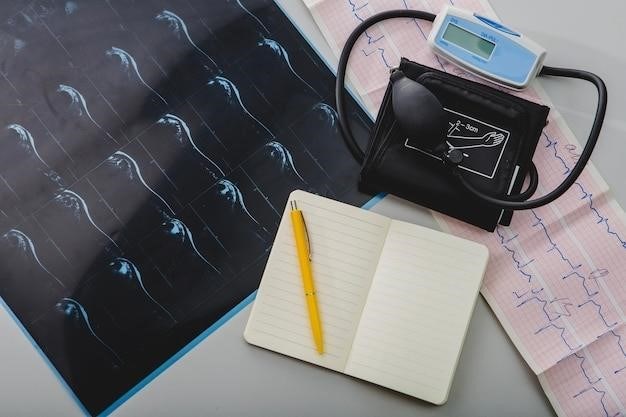
Electrocardiography (EKG or ECG) is a non-invasive, readily available tool that provides invaluable insights into the electrical activity of the heart․ An EKG traces the electrical impulses that control the heart’s rhythm and pumping action, revealing vital information about its health and function․ EKG interpretation is a fundamental skill for healthcare professionals, allowing them to diagnose and monitor a wide range of cardiac conditions․
A standard 12-lead EKG records electrical activity from multiple angles, providing a comprehensive view of the heart’s electrical activity․ Each lead represents a different view of the heart, capturing electrical signals from various regions․ The resulting waveform, known as an electrocardiogram, displays various waves, segments, and intervals, each representing a specific electrical event within the cardiac cycle․
Understanding EKG interpretation is essential for diagnosing and managing a variety of cardiac conditions, including arrhythmias, heart attacks, and heart failure․ Rapid interpretation of EKGs is crucial in emergency settings, where timely diagnosis and intervention can be life-saving․ This guide delves into the intricacies of EKG interpretation, equipping you with the knowledge and skills to decipher the language of the heart․
The Importance of Rapid EKG Interpretation
In the fast-paced world of healthcare, rapid and accurate EKG interpretation is not just a valuable skill but a crucial one, often making the difference between life and death․ The ability to quickly decipher the information presented on an EKG can significantly impact patient care, especially in emergency situations․
Imagine a scenario where a patient presents with chest pain․ A rapid EKG interpretation can quickly reveal whether the pain is caused by a heart attack or another condition․ This knowledge allows for immediate intervention, such as administering life-saving medications or initiating a cardiac catheterization procedure․ Early recognition of heart attacks and other cardiac emergencies is critical for improving patient outcomes․
Rapid EKG interpretation is not just about diagnosing acute events․ It also plays a crucial role in managing chronic cardiac conditions․ Regular EKG monitoring can help identify potential problems before they become serious, allowing for early intervention and prevention of complications․ This is especially important for individuals with heart failure, arrhythmias, or other heart conditions․ In essence, rapid EKG interpretation empowers healthcare professionals to make informed decisions and deliver timely, effective care․
Key Components of an EKG
An EKG, or electrocardiogram, is a recording of the electrical activity of the heart․ It provides a visual representation of the heart’s electrical impulses, which control the rhythm and function of the heart muscle․ Understanding the key components of an EKG is essential for accurate interpretation․
The standard EKG consists of 12 leads, each providing a different view of the heart’s electrical activity․ These leads are arranged in a specific pattern, and the resulting waveform is analyzed to identify any abnormalities․ The EKG waveform is typically divided into several segments, each representing a specific phase of the cardiac cycle․ These segments include the P wave, QRS complex, and T wave․
The P wave represents atrial depolarization, the electrical activation of the atria, which initiates the heartbeat․ The QRS complex represents ventricular depolarization, the electrical activation of the ventricles, which pumps blood out of the heart․ Finally, the T wave represents ventricular repolarization, the electrical recovery of the ventricles․ The morphology, duration, and timing of these components are crucial in determining the health of the heart and identifying any potential problems․
Common EKG Abnormalities
While a normal EKG reflects a healthy heart, various abnormalities can appear on the tracing, indicating potential cardiac issues․ Recognizing these abnormalities is crucial for timely diagnosis and treatment․ Some common EKG abnormalities include⁚
Arrhythmias⁚ These represent irregular heart rhythms, including tachycardia (fast heartbeat), bradycardia (slow heartbeat), and fibrillation (chaotic electrical activity)․ Arrhythmias can be caused by various factors, including heart disease, electrolyte imbalances, and medications․
Ischemia⁚ This refers to a reduced blood supply to the heart muscle, often due to narrowed coronary arteries․ EKG changes associated with ischemia include ST segment depression and T wave inversion․
Infarction⁚ This represents a heart attack, where the heart muscle is damaged due to prolonged lack of blood flow․ EKG changes associated with infarction include ST segment elevation, Q waves, and T wave inversion․
Hypertrophy⁚ This refers to an enlargement of the heart muscle, often due to high blood pressure or other conditions․ EKG changes associated with hypertrophy include increased QRS amplitude and axis deviation․
Understanding these common abnormalities allows healthcare professionals to quickly identify potential cardiac issues and initiate appropriate interventions․
Understanding EKG Rhythms
EKG rhythms, reflecting the electrical activity of the heart, are fundamental to EKG interpretation․ Understanding these rhythms allows healthcare professionals to assess the heart’s electrical conduction system and identify potential abnormalities․
The most common rhythm is the sinus rhythm, originating from the sinoatrial (SA) node, the heart’s natural pacemaker․ A normal sinus rhythm exhibits a regular heartbeat with a rate between 60 and 100 beats per minute․
Atrial fibrillation, a common arrhythmia, features irregular and rapid atrial activity․ The EKG shows chaotic atrial waves without distinct P waves, and the ventricular response is irregular․
Ventricular tachycardia is a serious arrhythmia characterized by rapid ventricular activity․ The EKG shows wide, bizarre QRS complexes, and the heart rate is typically above 100 beats per minute․
Atrial flutter presents with a rapid, regular atrial rhythm, often appearing as a “sawtooth” pattern on the EKG․ The ventricular response can be regular or irregular, depending on the conduction through the AV node․
Understanding these fundamental EKG rhythms is essential for healthcare professionals to accurately interpret EKG tracings and identify potential cardiac issues․
Recognizing Cardiac Ischemia and Infarction
EKG interpretation plays a vital role in detecting cardiac ischemia and infarction, conditions characterized by reduced blood flow to the heart muscle․ Identifying these conditions promptly is crucial for timely intervention and improved patient outcomes․
Ischemia, a temporary lack of oxygen, can manifest on the EKG as ST segment depression, T wave inversion, or both․ ST segment depression indicates a decrease in blood flow, while T wave inversion suggests prolonged ischemia․
Infarction, or a heart attack, occurs when blood flow to the heart muscle is completely blocked․ EKG changes associated with infarction include ST segment elevation, Q wave development, and pathological Q waves․
ST segment elevation is a hallmark of acute myocardial infarction (AMI) and signifies a critical reduction in blood flow․ Q waves, representing abnormal electrical activity in the infarcted area, can persist even after the acute event․
Recognizing these EKG changes is paramount for prompt diagnosis and treatment of cardiac ischemia and infarction․ Early intervention can significantly reduce the risk of complications and improve patient survival․
The Role of EKG in Emergency Medicine
In the fast-paced environment of emergency medicine, the EKG serves as a vital tool for rapid assessment and decision-making․ It provides a window into the electrical activity of the heart, allowing clinicians to quickly identify life-threatening conditions and guide immediate interventions․
For example, an EKG can detect a wide range of cardiac emergencies, including⁚
- Acute Myocardial Infarction (AMI)⁚ The EKG can reveal ST segment elevation, a hallmark of an ongoing heart attack, prompting immediate reperfusion therapy․
- Arrhythmias⁚ EKGs help identify dangerous heart rhythms, such as ventricular tachycardia or fibrillation, which require prompt treatment to prevent cardiac arrest․
- Pulmonary Embolism⁚ While not directly visualized on the EKG, the presence of right heart strain, such as right axis deviation or right ventricular hypertrophy, can suggest a pulmonary embolism․
The ability to rapidly interpret EKGs is essential for emergency medicine providers to make critical decisions regarding patient care, ensuring appropriate and timely treatment․
Advanced EKG Interpretation Techniques
While basic EKG interpretation provides a foundational understanding, advanced techniques allow for a more nuanced and comprehensive analysis․ These techniques involve a deeper understanding of EKG waveforms, their variations, and the subtle clues they can provide about cardiac function․
Here are some key advanced techniques⁚
- Quantitative EKG Analysis⁚ This involves using software to analyze EKG data, providing objective measurements of various parameters like heart rate variability, QT interval, and ST segment changes․ This can help identify subtle abnormalities that might be missed during visual inspection․
- Electrocardiographic Exercise Testing⁚ This involves performing an EKG during exercise, allowing clinicians to assess the heart’s response to stress and identify potential problems that may not be apparent at rest․
- Signal Averaging⁚ This technique involves averaging multiple EKG recordings to reduce noise and highlight subtle electrical abnormalities, such as ventricular late potentials, which are associated with an increased risk of sudden cardiac death․
Mastering these advanced techniques can significantly enhance the accuracy and clinical relevance of EKG interpretation, leading to better patient care and outcomes․
Case Studies and Practical Applications
To solidify your understanding and build confidence in rapid EKG interpretation, it’s crucial to apply your knowledge to real-world scenarios․ Case studies provide valuable learning opportunities by presenting complex EKG patterns and clinical situations, challenging you to analyze the findings and make informed decisions․
Here are some practical applications of rapid EKG interpretation⁚
- Emergency Medicine⁚ In emergency settings, rapid EKG interpretation is essential for quickly diagnosing and managing life-threatening conditions like myocardial infarction, arrhythmias, and pericarditis․
- Cardiology⁚ Cardiologists rely on EKGs to assess the heart’s electrical activity, diagnose and monitor heart disease, and guide treatment decisions․
- Primary Care⁚ EKGs can be a valuable tool in primary care for detecting early signs of heart disease, monitoring patients with known heart conditions, and identifying risk factors for cardiovascular disease․
- Sports Medicine⁚ EKGs are used to assess the cardiovascular health of athletes, identify potential risks, and guide training programs;
By working through case studies and applying your knowledge in real-world settings, you’ll gain valuable experience and develop the skills necessary for confident and accurate EKG interpretation․
Conclusion and Future Directions
Rapid EKG interpretation is an essential skill for healthcare professionals, enabling them to quickly assess cardiac function, diagnose heart conditions, and make timely treatment decisions․ The ability to accurately interpret EKGs is crucial in various clinical settings, including emergency medicine, cardiology, primary care, and sports medicine․
As technology continues to advance, we can expect further developments in EKG interpretation․ Artificial intelligence (AI) is increasingly being used to analyze EKG data, providing insights and support for clinicians․ AI-powered EKG interpretation tools can help to improve accuracy, efficiency, and patient care․
Future directions in EKG interpretation may also include the development of novel EKG techniques and the integration of EKG data with other diagnostic tools․ As our understanding of the heart’s electrical activity grows, so too will our ability to use EKGs to diagnose and manage cardiac conditions effectively․
In conclusion, rapid EKG interpretation is a vital skill for healthcare professionals, empowering them to make informed decisions and provide optimal patient care․ As technology continues to evolve, we can anticipate exciting advancements in EKG interpretation, further enhancing our ability to understand and treat heart disease․